Lung Cancer Causes
The most common cause of lung cancer is smoking. This can result from the patient smoking or being exposed to second-hand smoke. Smoking damages the cells in the lining of the lungs and causes tissue to change almost immediately upon inhalation. After repeated exposure to smoke, the cells in the lungs begin to act abnormally and cancer may develop.
In addition to smoking, other risk factors for lung cancer include:
- Repeated exposure to radon gas, asbestos, air pollution or other carcinogens
- Chronic lung disease
- Family history of lung cancer
Although there is no guaranteed method for preventing lung cancer, risk may be reduced by:
- Never smoking
- Quitting if you smoke
- Staying away from second-hand smoke
- Avoiding carcinogens
- Testing your home for radon
- Eating a healthy diet and exercising regularly
Lung Cancer Symptoms
In its early stages, lung cancer often doesn’t cause noticeable symptoms.
Symptoms typically aren’t apparent until the condition advances and may include:
- A cough that doesn’t go away or gets worse
- Shortness of breath
- Hoarseness
- Chest pain
- Coughing up blood
- Frequent lung infections
Once cancer has spread, other symptoms may appear including:
- Unexplained weight loss
- Headaches
- Bone pain
Surgical Treatment Options
Surgery is most often considered for early-stage non-small cell lung cancers (NSCLC). When the cancer is localized and has not spread, this treatment option may provide the best chance to cure the disease. But surgery is not always an option for treating lung cancer. Each case must be carefully considered based on a number of options.
If it is determined that a patient with lung cancer would benefit from lung cancer surgery, there are a variety of procedures that may be performed. The type of surgery will depend on the size, location, and stage of the cancer, as well as a patient’s overall health.
Options for lung cancer surgery include:
Risks of Lung Cancer Surgery
All surgery involves some risk. The most common risks associated with lung cancer surgery include:
- Bleeding
- Infection
- Collapse of the lung
- Pneumonia
- Damage to nearby structures
- Blood clots
- Reaction to anesthesia
What to Expect After Surgery
Following lung cancer surgery, patients spend some time in the hospital. The length of time depends upon the type of procedure performed, as well as the patient’s overall health status, age, and need for post-surgical care (5 to 7 days is typical). After surgery, most patients initially stay in the intensive care unit (ICU) where their vital signs are closely monitored. They are then moved to a regular patient room when it is deemed safe to do so. When able, patients will be encouraged to sit up and walk around in order to regain strength and reduce the risk of blood clots. About 3 to 4 days after surgery, the chest tube placed to drain fluid during and after surgery will be removed.
Once home, patients may gradually return to their daily activities. The timeframe for this will be based on the type of procedure performed, the patient’s general health and energy levels, and specific doctor recommendations. If the procedure is done using a thoracotomy, activity may be limited for at least a month or two.
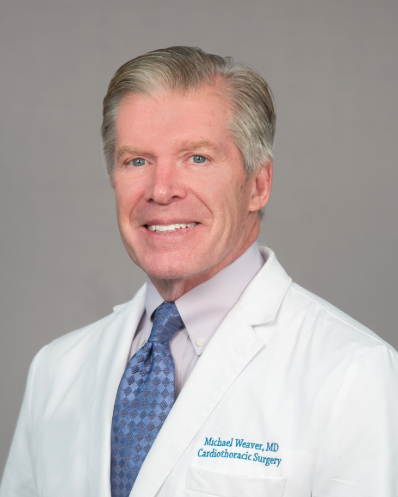
Become a Patient
Call (225) 763-4457 to speak to our patient navigator.